Round-Celled Sarcoma
Description
This section is from the book "Cancer And Other Tumours Of The Stomach", by Samuel Fenwick. Also available from Amazon: Cancer and other tumours of the stomach.
Round-Celled Sarcoma
This variety is the one most usually met with, and was observed in thirty-three out of fiftythree cases, or in about 62 per cent, of the entire number. As a rule, it occurs in the form of a dense infiltration of the pyloric third of the stomach, which transforms the coats of this portion of the viscus into a homogeneous yellowish-white mass of rigid consistence and considerable thickness. The peritoneal aspect is often covered with lymph, while the inner surface is slightly uneven, or even distinctly nodular, and is occasionally superficially ulcerated. If the pylorus is greatly thickened, its orifice may be partially stenosed, as in cases of spheroidal-celled carcinoma ; but as a rule the rigidity of its tissues renders it patent and the valve incompetent rather than contracted. The growth gradually shades off towards the centre of the organ, but it is often prolonged for some distance along the curvatures in the form of thick striae or bands. In almost every instance, whether the pylorus is stenosed or not, the cardia is dilated and its mucous membrane shows signs of chronic inflammation. In about one-sixth of the cases the entire organ was infiltrated by the growth, which also tended to invade the lower end of the oesophagus and the first portion of the duodenum. The walls of the stomach were greatly thickened and. its cavity contracted, while in some instances the inner surface presented extensive superficial ulceration. In only two cases out of the entire number did the disease occur as a circumscribed tumour in the wall of the viscus, with secondary nodules in the surrounding mucous membrane.
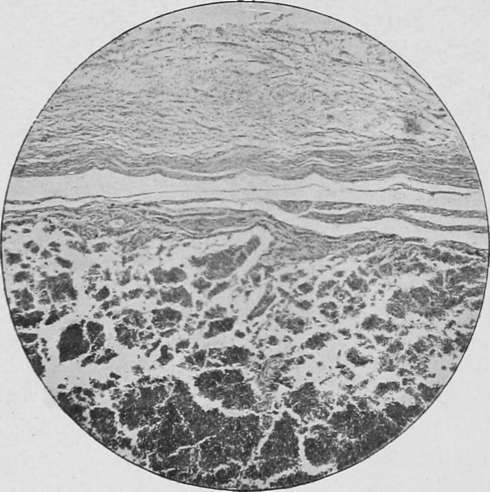
Fig. 54.- Section of a stomach showing round-cell infiltration of the submucosa (sarcoma). ( x 100.).
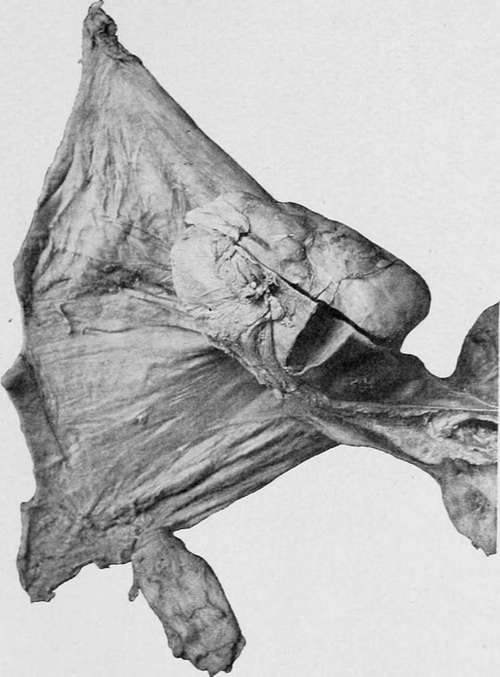
Fig. 55.-A spindle-celled sarcoma, the size of a small potato, attached to the fundus of the stomach and the gastro-splenic omentum. (London Hospital Museum.).
Continue to:
- prev: Part II. Tumours Of The Stomach And Duodenum. Chapter I. Sarcoma Of The Stomach
- Table of Contents
- next: Spindle-Cell Or Fibro-Sarcoma